IBD Treatment & Why Nutrition is Important
Following on from last week’s blog explaining the tests involved in the diagnosis of IBD, next comes treatment and management once a diagnosis has been given.
Inflammatory Bowel Diseases are chronic, relapsing conditions for which there is currently no cure, but there are a variety of different medications that play an important role at helping to induce and achieve remission (get us well) and maintain remission (keep us well). Nutrition support alongside these is so important and can help to reduce side effects, manage symptoms, and improve quality of life.
IBD Treatment Pyramid & Why Nutrition is Important
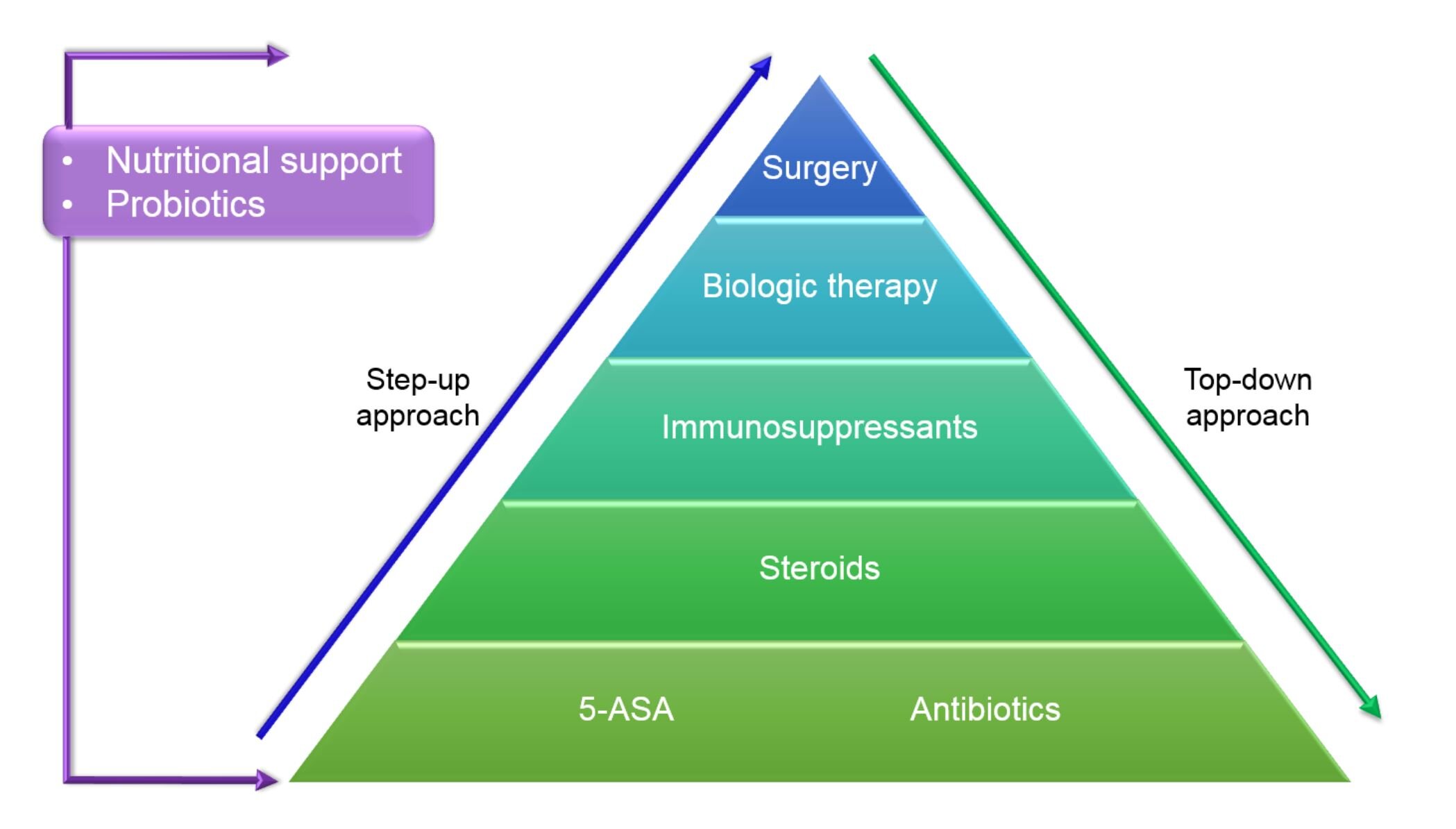
The pyramid below shows the main IBD medication categories. Gastroenterologists will decide which is the best route to take based on the type of IBD we have, the severity of the inflammation, our age and other factors. Traditionally a ‘step up’ approach has been taken, starting at the bottom and working up but in some cases gastroenterologist may decide to start further up or take a ‘top down approach’.
Aloi, et al. (2014). https://doi.org/10.1038/nrgastro.2013.158
Alongside any of the medical approaches that we will discuss below, as can be seen in the pyramid, nutritional support is important. It helps to give medication the best chance of success. Nutritional support can hugely help improve symptoms and quantity of life, and may help reduce the number of relapses and risk for other diseases (1). Some of the medications used to treat IBD may also impact our ability to absorb and use certain nutrients (e.g. sulfasalazine and folate) so again this is why nutrition support alongside medical treatment is so important.
IBD Medications
5-ASAs or Aminosalicylates
Examples:
Sulfasalazine (Azulfidine®, Salazopyrin)
Mesalazine – Pentasa, Salofalk, Ipocol.
Mesalamine - Asacol® HD, Pentasa®, Mezavant/Lialda™, Apriso®, Delzicol™
Olsalazine (Dipentum®)
Balsalazide (Colazal®)
Canasa® - suppositories
Rowasa® - Enema formulations
What they do: prevent the production and secretion of inflammatory mediators at the level of the gut lining. They are most effective in the colon and are typically prescribed as tablets (delayed release) or can be inserted rectally (suppositories or enemas).
When they are used: Used in Crohn’s disease or ulcerative colitis, but are often more effective in ulcerative colitis. They have been shown to independently induce and maintain remission in mild to moderate ulcerative colitis. In Crohn’s disease, they may also be helpful to control mild inflammation and symptoms. However, recent research suggests that they often need to be used in conjunction with other therapies to adequately control inflammation and prevent complications in Crohn’s disease (2).
Why nutrition is important: sulfasalazine impacts the absorption and metabolism of folate so adequate nutritional support needs to be considered (3).
Antibiotics
Examples:
Metronidazole
Ciprofloxacin
What they do: treat bacterial infections.
When are they used: may be used for Crohn's disease and UC in certain circumstances such as those with perianal disease or abscesses. Also used to treat pouchitis (2).
Why nutrition is important: although they do a great job of getting rid of the bad guys; they also reduce and impact the good guys too – the trillions of helpful bacteria that live in our gut (microbiota) so nutritional and, in some cases, probiotic support, can be really important in helping to reduce antibiotic associated diarrhoea and support the microbiota during and after probiotics.
Corticosteroids
Examples:
prednisolone (brand names Deltacortril®, Deltastab® and Dilacort®)
prednisone
hydrocortisone (Plenadren®)
methylprednisolone (Medrone®)
beclometasone dipropionate (Clipper®)
budesonide (Entocort® and Budenofalk®)
budesonide-MMX (Multi-Matrix system) (Cortiment®) (4)
What they do: decrease the activity of the immune system which decreases inflammation.
When are they used: They are prescribed short-term to control flares and help bring inflammation under control (2). Prednisone circulates throughout the entire body (systemic action), whereas budesonide works locally and therefore has fewer side effects (5).
Why nutrition is important: side effects of prednisone can include increased appetite, weight gain and insulin resistance but nutrition support alongside taking them may help mitigate these. Prednisone can also have an impact on bone health and bone density so nutritional support to reduce bone loss and osteoporosis is important (6).
Immunomodulators
Examples:
6-mercaptopurine (6- MP, Purinethol®),
Azathioprine (Imuran®, Azasan®)
Methotrexate (MTX®, Rheumatrex®, Mexate®)
Tacrolimus (Prograf®)
Cyclosporine A (Sandimmune®, Neoral®)
What they do: modify the activity of the immune system which decreases the inflammatory response.
When are they used? In both UC and Crohns, typically when 5 ASA’s have failed or been ineffective and in moderate to severe disease.
Why nutrition is important: methotrexate impacts the absorption and metabolism of folate so adequate nutritional support needs to be considered (7).
Biologics
Examples
Anti-tumour necrosis factor α (TNF-α) agents - Adalimumab (Humira®), Infliximab (Remicade®), Certolizumab pegol (Cimzia)
Integrin Receptor Antagonists - Vedolizumab (Entyvio™)
Interleukin-12 and -23 Antagonist - Ustekinumab (Stelara®)
What do they do? they stop the body's ability to produce specific inflammatory proteins (TNFs, integrins, interleukins etc.).
When are they used? They are typically prescribed for moderate to severe cases of Crohn's and UC and where other treatments have not worked.
Why is nutrition important: helping to support and reduce symptoms whilst the biologics work, helping to reduce extra intestinal symptoms and correct nutritional deficiencies, supporting gut and overall health and improving quality of life.
JAK Inhibitors
Examples;
Tofacitinib (Xeljanz)
Filgotinib (Jyseleca)
What do they do? Work directly on the immune system to interfere with and block pathways that lead to inflammation.
When are they used? Moderate to severe UC. Also being trialled in Crohn’s Disease.
Why is nutrition important: helping to support and reduce symptoms, helping to reduce extra intestinal symptoms, correct nutritional deficiencies, support gut and overall health and improve quality of life.
If you’d like help with your IBD, lets have a chat. You can book a (free) 20 minute no obligation phone call with me to find out how I can help you. During this call I’d love to hear about you; your journey, your struggles, your life, and we can chat about the best route forward for you. Whether you are right at the beginning of your journey or have had IBD for years I can help.
If that sounds interesting click below and find a time that works for you.
Disclaimer: All content found on the nalmclinic.com website, including: text, video, or other formats have been created for informational purposes only. The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your doctor, consultant or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
We are all wonderfully unique and what works for one person may not work for another so please seek help and advice before changing your diet to work out the right way forward for you.
References
Haskey, N., & Gibson, D. L. (2017). An Examination of Diet for the Maintenance of Remission in Inflammatory Bowel Disease. Nutrients, 9(3), 259. https://doi.org/10.3390/nu9030259
Lamb CA, Kennedy NA, Raine T, et al (2019) British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut;68:s1-s106.
Halsted CH, Gandhi G, Tamura T. Sulfasalazine inhibits the absorption of folates in ulcerative colitis. N Engl J Med. 1981 Dec 17;305(25):1513-7. doi: 10.1056/NEJM198112173052506. PMID: 6117796.
Crohns and Colitis UK (2021) Steroids. Available at: https://www.crohnsandcolitis.org.uk/about-crohns-and-colitis/publications/steroids, (Accessed 14th July 2021)
Campieri M, Ferguson A, Doe W, et al. Oral budesonide is as effective as oral prednisolone in active Crohn’s disease. Gut 1997;41:209-214.
Lima, C. A., Lyra, A. C., Rocha, R., & Santana, G. O. (2015). Risk factors for osteoporosis in inflammatory bowel disease patients. World journal of gastrointestinal pathophysiology, 6(4), 210–218. https://doi.org/10.4291/wjgp.v6.i4.210
Herfarth, H. H., Kappelman, M. D., Long, M. D., & Isaacs, K. L. (2016). Use of Methotrexate in the Treatment of Inflammatory Bowel Diseases. Inflammatory bowel diseases, 22(1), 224–233. https://doi.org/10.1097/MIB.0000000000000589