Vitamin D and IBD
What is Vitamin D?
Vitamin D plays many roles in the body, such as regulating the amount of calcium and phosphate and is essential for bone health. It also helps reduce inflammation and therefore key to good overall health and growth.
How much Vitamin D do we need?
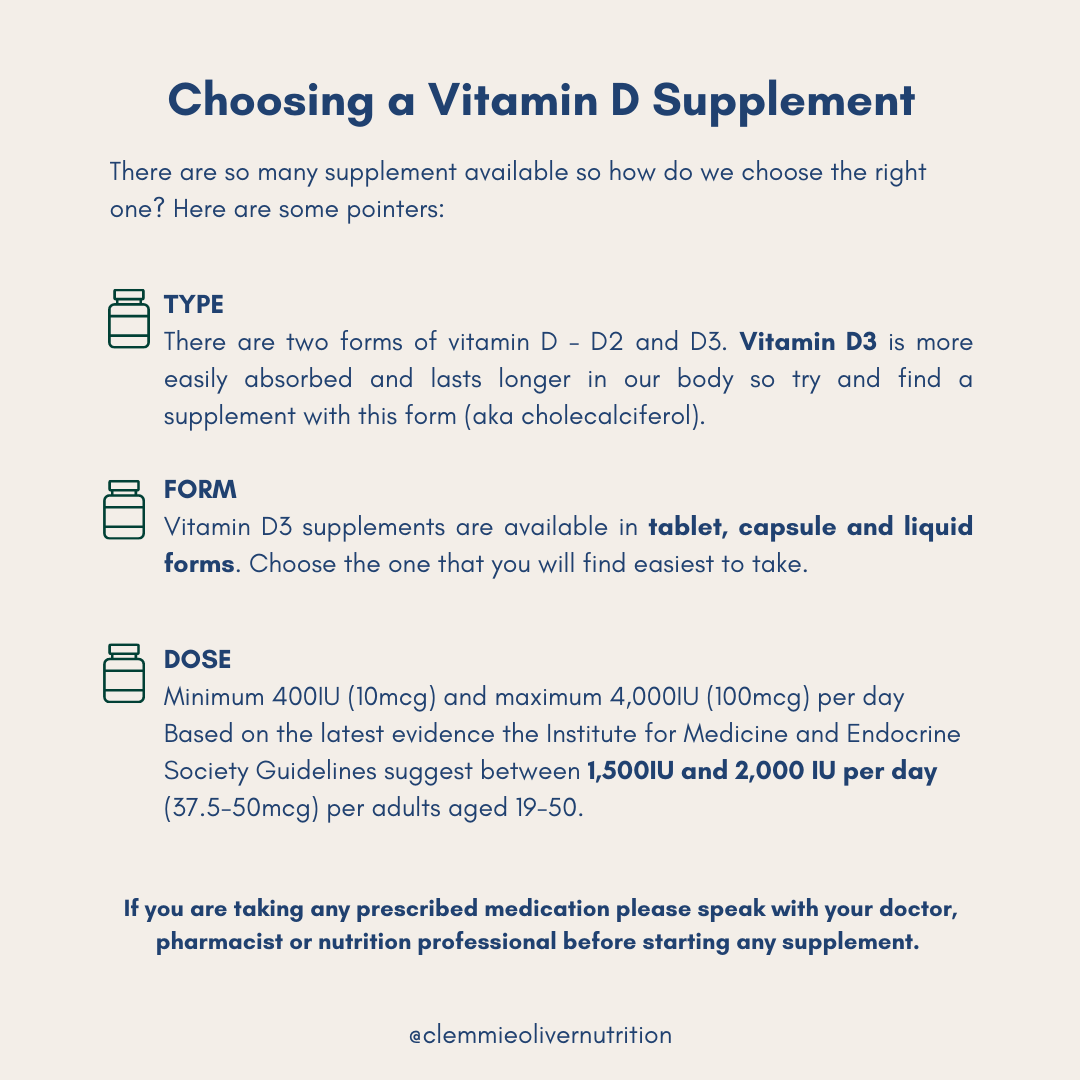
NHS guidelines suggest adults need 10mcg (400IU) per day of vitamin D (1).
There is some discussion at the moment as to whether these recommendations need to be updated. They are based on the recommended daily allowance (RDA) figures which were published in 1941 but we have learnt so much more about vitamin D since then.
The Institute of Medicine and Endocrine Practice Guidelines Committee suggest 1500-2000IU per day may be more appropriate based on more recent evidence (2). The safe upper limit for vitamin D intake is 100mcg (4000IU) per day for adults over 18. It is really important that you do not take any more than this unless suggested by your medical or nutrition team as high than this dose is considered medically unsafe.
Prevalence of vitamin D deficiency in IBD
Different studies show varied prevalence of vitamin D deficiency in IBD, but in some studies around 60-70% of people with IBD have insufficient vitamin D levels. However, this statistic depends on numerous factors like location of study - as some places may not get as much sun as other places around the world, season of measurement and the proportion of people that have active IBD or are in remission (3). Some evidence shows that prevalence of vitamin D deficiency is higher in people with Crohn’s Disease than with Ulcerative Colitis (4). The reasons for this remain unclear but include lack of sun exposure due to immune-suppressive treatments, dietary restrictions, and impaired absorption of nutrients (5).
Research study: Vitamin D and IBD (2016) (5)
This study was done by The University of Pittsburgh where a total of 965 IBD patients had their vitamin D levels monitored for 5 years, along with their clinic status that was based on IBD-related markers. They found that low vitamin D levels were common in IBD patients and were associated with higher morbidity and disease severity, highlighting the importance of vitamin D monitoring and treatment.
Symptoms of vitamin D deficiency
Tiredness
Aches and pains
Bone deformities
Bone pain and tenderness
People with IBD are at a higher risk of developing osteoporosis and part of this is due to the lack of vitamin D as it is essential for calcium absorption.
Why is it more likely for me to be vitamin D deficient if I have IBD?
- Reduced exposure to the sun - as a result of symptoms during a flare up or during active disease, we may tend to stay inside, resting or feel unable to go out due to poor access to a toilet. Due to some medications people with IBD may not expose themselves to direct sunlight to protect against the harmful effects of sun exposure.
- People living in certain areas of the world that may get less sunlight than others are at a greater risk of having a vitamin D deficiency.
- Vitamin D is a fat soluble vitamin and people with active inflammation in the small intestine poorly absorb fat, hence poorly absorb vitamin D.
How do I get Vitamin D?
From the sun, food and supplements.
Vitamin D is made under our skin, as a result of a reaction to sunlight, hence increasing sun exposure can help increase vitamin D levels. However, this must be done safely and avoid too much exposure which can cause burns and this also may not be possible or safe for some people with IBD who may be on medications that increase their risk of skin cancers.
Below are some foods rich in vitamin D but these may not be adequate enough to support our intake on their own:
- Oily fish: salmon, sardines and mackerel
- Eggs
- Beef liver
- Cheese
- Mushrooms
If you can, please get tested before with your GP or IBD team to see whether you are deficient. If you do supplement yourself, please ensure it is well within the recommended dose and always consult your doctor/GP before starting a new supplement. The safe upper limit for vitamin D intake is 100mcg (4000IU) per day for adults over 18. It is really important that you do not take any more than this unless suggested by your medical or nutrition team as high than this dose is considered medically unsafe.
If you want support with your diet, nutrition and IBD journey we can help.
At The NALM Clinic we have an IBD specialist Nutritional Therapist (Clemmie) and specialist gastroenterology Dietician (Jess) and and we are here to support you. We both have IBD too so we ‘get it’ and are so passionate about helping others.
If you would like support with your IBD please book a call with me via the button below.
Disclaimer: All content found on the nalmclinic.com website, including: text, video, or other formats have been created for informational purposes only. The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your doctor, consultant or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
We are all wonderfully unique and what works for one person may not work for another so please seek help and advice before changing your diet to work out the right way forward for you.
References
Vitamin D [Internet]. nhs.uk. 2020 [cited 27 May 2022]. Available from: https://www.nhs.uk/conditions/vitamins-and-minerals/vitamin-d/
Michael F. Holick, Neil C. Binkley, Heike A. Bischoff-Ferrari, Catherine M. Gordon, David A. Hanley, Robert P. Heaney, M. Hassan Murad, Connie M. Weaver, Evaluation, Treatment, and Prevention of Vitamin D Deficiency: an Endocrine Society Clinical Practice Guideline, The Journal of Clinical Endocrinology & Metabolism, Volume 96, Issue 7, 1 July 2011, Pages 1911–1930, https://doi.org/10.1210/jc.2011-0385
Ananthakrishnan AN. Vitamin D and inflammatory bowel disease. Gastroenterology & Hepatology. 2016 Aug;12(8):513.
Fletcher J, Swift A. Vitamin D screening in patients with inflammatory bowel disease. Gastrointestinal Nursing. 2017 Nov 2;15(9):16-23.
Fletcher J, Cooper SC, Ghosh S, Hewison M. The role of vitamin D in inflammatory bowel disease: mechanism to management. Nutrients. 2019 May;11(5):1019.
Kabbani TA, Koutroubakis IE, Schoen RE, Ramos-Rivers C, Shah N, Swoger J, Regueiro M, Barrie A, Schwartz M, Hashash JG, Baidoo L. Association of vitamin D level with clinical status in inflammatory bowel disease: a 5-year longitudinal study. Official journal of the American College of Gastroenterology| ACG. 2016 May 1;111(5):712-9.